From COVID-19 to malaria: Six applications of peptide microarrays in infectious diseases
Article
In recent years, researchers have used peptide microarrays to explore everything from vaccine response and viral variant tracking to diagnostic marker discovery across a range of diseases, including COVID-19, malaria, leishmaniasis, schistosomiasis, and African Swine Fever.
This article highlights six recent studies where peptide microarrays played a central role. Each case shows how the technology can uncover hidden immunological insights, challenge vaccine design assumptions, or accelerate diagnostic development. Whether probing why certain vaccine candidates underperform or revealing conserved viral regions ideal for broad protection, peptide microarrays are shaping how we fight infectious diseases at the molecular level.
1. Defining the antibody response to the malaria vaccine candidate MSP2
Overview: A study led by scientists at the Karolinska Institute investigated how the human immune system naturally responds to Plasmodium falciparum Merozoite Surface Protein 2 (MSP2), a protein considered for use in a malaria vaccine. Specifically, the researchers focused on whether naturally acquired IgG antibodies target the conserved N- and C-terminal regions of MSP2. Using samples from malaria-infected travelers and individuals living in malaria-endemic Tanzania, the team found that while immune responses were robust against the highly variable central part of MSP2, there was little to no naturally occurring antibody recognition of the conserved termini. Structural modeling suggested that the conserved regions may be structurally hidden or variable, which could explain the lack of immune targeting.
Why this matters: The findings challenge prior assumptions that conserved regions of antigens like MSP2 are naturally immunogenic and thus ideal vaccine targets. Most malaria vaccine strategies aim to induce broad protection by targeting conserved sequences, under the assumption that they would generate cross-strain immunity. However, this study reveals that natural infection does not efficiently generate antibodies against these conserved MSP2 domains. This has significant implications for vaccine development: to be effective, vaccines may need to target the more variable, yet naturally immunodominant, regions of MSP2 or include multiple antigen variants to broaden protection.
How peptide microarrays were used: To map the antibody binding sites with high resolution, the researchers employed a custom PEPperCHIP® Peptide Microarray developed by PEPperPRINT. This microarray featured 128 overlapping 13-amino acid peptides derived from 494 unique MSP2 variants. It allowed the team to detect whether IgG antibodies from infected individuals recognized linear epitopes within the conserved N- and C-termini of MSP2. While ELISA tests showed little to no antibody response to full-length or peptide versions of the conserved regions, the PEPperCHIP® microarray did detect limited, individual-specific binding to some linear epitopes in these regions. This demonstrated that while certain conserved epitopes might be theoretically accessible, they are rarely targeted by the natural immune response, likely due to structural conformation or epitope masking on the parasite surface.
Reference: Zerebinski et al., “Naturally acquired IgG responses to Plasmodium falciparum do not target the conserved termini of the malaria vaccine candidate Merozoite Surface Protein 2”. Frontiers in Immunology. (2024 December).
https://doi.org/10.3389/fimmu.2024.1501700
2. Designing a custom antigen for the diagnosis of Canine Visceral Leishmaniasis
Overview: Researchers at the Universidade Federal de Viçosa in Brasil designed a study aiming at improving diagnostic tools for canine visceral leishmaniasis (CVL), a disease caused by Leishmania infantum that affects dogs and poses a risk to human health. The researchers used a high-resolution peptide microarray to map linear epitopes on the LiNTPDase2 antigen. They identified six positive epitopes and four negative (cross-reactive) ones. Three of the positive peptides (NT2_1, NT2_3, NT2_6) showed strong performance in ELISA tests, and their combination (MIX3) achieved 97.58% diagnostic accuracy. Additionally, by removing the negative epitopes, the researchers engineered an optimized antigen (rNT2.neg), which significantly improved specificity and reached 93.07% accuracy in a large sample set.
Why this matters: Current tests for CVL often suffer from poor specificity due to cross-reactions with other diseases like Chagas. This leads to misdiagnoses and undermines disease control programs. By precisely mapping immune-reactive regions and redesigning the diagnostic antigen, this study delivers both a highly accurate peptide combination and a new, refined protein antigen. These findings support the development of more accurate, specific, and field-adaptable diagnostic assays, which are essential tools for disease monitoring, control, and potential elimination efforts in endemic regions.
How peptide microarrays were used: A custom PEPperCHIP® Peptide Microarray was used to screen 375 overlapping peptides spanning the LiNTPDase2 protein. The array was tested against pooled sera from CVL-positive, CVL-negative, and Chagas-infected dogs. Fluorescence-based detection identified specific antibody-binding patterns, enabling the researchers to distinguish peptides uniquely reactive to CVL and exclude those prone to cross-reactivity. This high-resolution epitope mapping was key to both peptide selection and the design of the optimized rNT2.neg antigen.
Reference: Castro et al. “High-resolution mapping of linear epitopes from LiNTPDase2: Advancing leishmaniasis detection using optimized protein and peptide antigens”. Diagnostic Microbiology and Infectious Disease. (2024 October).
https://doi.org/10.1016/j.diagmicrobio.2024.116448
3. Developing a new diagnostic method for schistosomiasis
Overview: A study published by scientists from two universities in Zimbabwe aimed to identify antibody-detectable markers (B-cell epitopes) for schistosomiasis caused by Schistosoma haematobium and S. mansoni. Researchers used computational tools to predict short protein segments likely to trigger immune responses, and then validated these predictions using a peptide microarray. Among 122 peptides tested, 10 showed good or acceptable ability to distinguish infected individuals from uninfected controls. One peptide, AAB81008-19-30, stood out with strong diagnostic performance for both parasite species. Several others showed acceptable performance, especially for detecting S. mansoni. However, fewer peptides showed reliable performance for S. haematobium, highlighting the challenge of species-specific diagnosis.
Why this matters: Schistosomiasis affects over 200 million people globally and is often underdiagnosed due to limitations in existing tests, especially in early or low-burden infections. This research demonstrates a promising approach for developing more sensitive, species-specific serological tests. These tests could be especially impactful in resource-limited settings, where conventional microscopy is impractical or insensitive. Moreover, some of the identified peptides may help detect early-stage infections that would otherwise go unnoticed.
How peptide microarrays were used: PEPperPRINT’s peptide microarrays were used to experimentally test which predicted peptides are recognized by antibodies in patient sera. The arrays displayed all 122 candidate peptides, and fluorescence signals were measured after incubation with sera from infected and uninfected individuals. This high-throughput setup allowed the researchers to simultaneously test the diagnostic potential of dozens of peptides and identify those that best differentiated infected individuals from healthy or uninfected ones.
Reference: Vengesai et al., “Identification of Schistosoma haematobium and Schistosoma mansoni linear B-cell epitopes with diagnostic potential using in silico immunoinformatic tools and peptide microarray technology”. PLOS Neglected Tropical Diseases. (2024 August).
https://doi.org/10.1371/journal.pntd.0011887
4. Measuring the immune response of different SARS-CoV-2 vaccine approaches
Overview: Researchers in Denmark investigated how different combinations of DNA vaccines influence the immune response to SARS-CoV-2 in mice. Researchers compared three groups: mice vaccinated with a DNA vaccine encoding the original spike protein (Index strain), the Beta variant spike, or a combination of both (heterologous regimen). Using antibody profiling, they found that the heterologous regimen produced a distinct antibody response, targeting additional regions of the spike protein not strongly recognized in the other groups. These included specific regions in the SD2 and HR2 domains—areas of the virus believed to be functionally important and more conserved. This broader targeting may help explain the increased neutralization breadth observed with the mixed vaccine approach.
Why this matters: SARS-CoV-2 variants continue to evolve, often escaping immunity from earlier vaccines. A key goal in vaccine development is to stimulate antibodies that recognize conserved regions, meaning parts of the virus that don't change much and are crucial to its function. This study shows that mixing antigens from different variants in a prime-boost strategy can shift the immune response toward such conserved regions. It provides insight into how vaccine design can be fine-tuned to improve cross-variant protection, an important step toward future-proofing vaccines against evolving viruses.
How peptide microarrays were used: The researchers used a custom peptide microarray from PEPperPRINT to map antibody binding sites at high resolution. The array included overlapping cyclic peptides spanning the SARS-CoV-2 spike protein and key variant mutations. By testing pooled sera from each vaccine group, they identified which regions were most strongly targeted. This technology enabled precise comparison of immune responses across vaccination strategies and revealed that heterologous vaccination uniquely boosted recognition of the SD2 and HR2 regions.
Reference: Frische et al. “Antigen-Heterologous Vaccination Regimen Triggers Alternate Antibody Targeting in SARS-CoV-2-DNA-Vaccinated Mice”.Vaccines. (2024 February).
https://doi.org/10.3390/vaccines12030218
5. Identifying vaccine targets for the African Swine Fever Virus
Overview: A study developed by scientists from the Joint Research Centre in Italy aimed to identify antibody-binding regions on the African Swine Fever Virus (ASFV) to support vaccine and diagnostic development. Researchers analyzed serum from pigs infected with various ASFV strains using a high-density peptide microarray covering 12 viral proteins. The array revealed several proteins—such as p12, p54, B646L (p72), D117L (p17), and E120R—as strongly reactive, with specific peptide sequences consistently recognized by antibodies. These included known immunogenic regions and new candidate epitopes. Despite individual variation among samples, some peptides were commonly recognized and could serve as targets for future ASF vaccines or diagnostic assays.
Why this matters: ASF is a highly contagious and deadly disease with no approved vaccine. Progress in vaccine development has been slow, partly because the virus's protective antigens—viral proteins that elicit strong immune responses—are still poorly understood. This study helps close that gap by identifying which parts of the virus are most consistently recognized by the pig immune system. These findings not only advance the search for effective vaccine components but also support improved, antibody-based diagnostics.
How peptide microarrays were used: The study used a custom PEPperCHIP® Peptide Microarray displaying 5,410 overlapping 15-amino acid peptides from 12 ASFV proteins. Pig sera were applied to the chip, and antibody binding was detected using fluorescence scanning. This high-resolution epitope mapping enabled the team to pinpoint precise regions recognized by antibodies across different ASFV strains. The microarray’s throughput and sensitivity allowed efficient screening and comparison of multiple viral proteins and serum samples in parallel.
Reference: Desmet et al. “ASFV epitope mapping by high density peptides microarrays”. Virus Research. (2024 January).
https://doi.org/10.1016/j.virusres.2023.199287
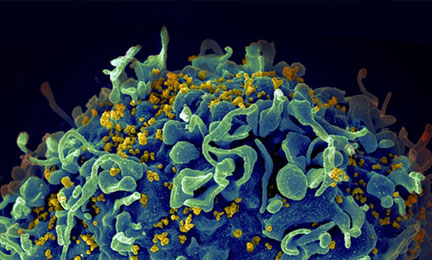
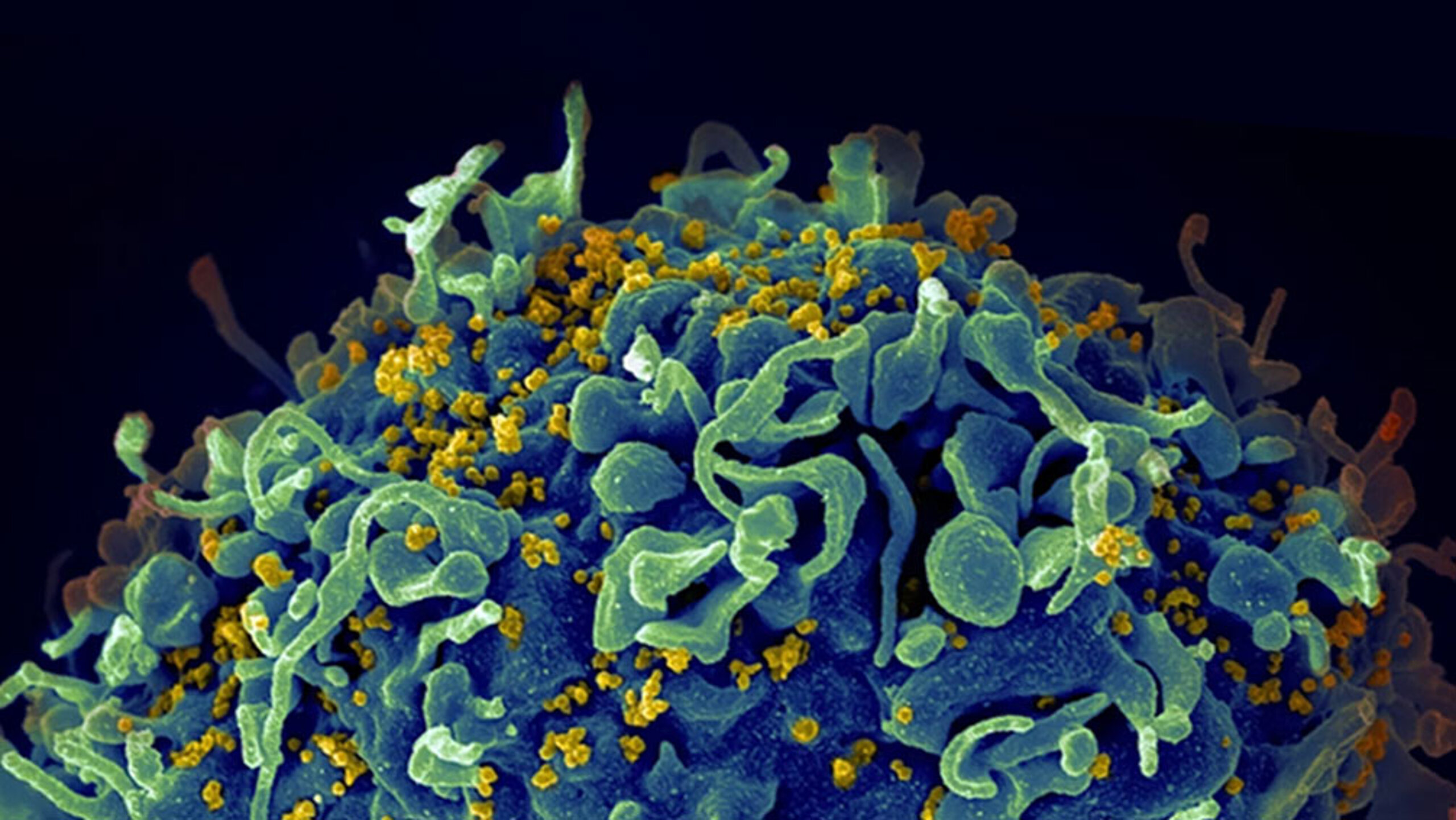
6. Mapping antibody responses to variations of the HIV fusion peptide
Overview: Researchers at the American NIH tested 17 different vaccine regimens in mice to explore how to best generate broadly neutralizing antibodies against the HIV-1 fusion peptide (FP), a vulnerable site on the virus. By altering FP length and carrier proteins (which help trigger an immune response) during priming and boosting with diverse HIV Env trimers (containing the full HIV spike protein), researchers identified four distinct classes of antibodies: two previously known and two newly discovered. Some regimens led to significantly stronger and broader antibody responses. Notably, varying FP length during priming improved neutralization in both mice and guinea pigs. Collectively, the antibodies neutralized over 50% of a 208-strain HIV panel, a promising result for HIV vaccine design.
Why this matters: HIV mutates rapidly, making it difficult to create a vaccine that works across all strains. However, the fusion peptide is a relatively stable target. This study shows that by tweaking how we present this part of the virus to the immune system—specifically by varying its length and delivery method—we can train the body to produce more effective antibodies. It also highlights that different antibody “types” can target the same site in unique ways, giving researchers more tools to design vaccines that protect against a broader range of HIV variants.
How peptide microarrays were used: The team used the PEPperMAP® epitope mapping to analyze how each antibody class recognized different FP sequences. The microarray included substitution variants of the FP to test how changes at each position affected antibody binding. This helped define the sequence preferences and tolerances of each antibody class, clarifying why some antibodies had broader neutralization than others. It was instrumental in understanding how structural recognition relates to antibody function.
Reference: Sastry, et al. “Diverse Murine Vaccinations Reveal Distinct Antibody Classes to Target Fusion Peptide and Variation in Peptide Length to Improve HIV Neutralization.” Journal of Virology. (2023 April).
https://doi.org/10.1128/jvi.01604-22
How peptide microarrays can support your infectious disease research
With unmatched precision, flexibility, and throughput, PEPperPRINT helps researchers map antibody epitopes, profile immune responses, and identify diagnostic or vaccine-relevant biomarkers faster and with greater resolution.
Whether you're studying immune responses to viral variants, validating vaccine candidates, or identifying serological markers for neglected tropical diseases, PEPperPRINT’s peptide microarray platform delivers the high-resolution data you need to move from discovery to application.
Contact PEPperPRINT today to explore how peptide microarrays can accelerate your infectious disease research and improve outcomes in diagnostics and vaccine development.